
A balanced approach to supplementation can enhance overall well-being for those living with schizophrenia.
Introduction
Could a simple vitamin deficiency be linked to a complex condition like schizophrenia? Research indicates that individuals with schizophrenia often have lower levels of key nutrients, such as vitamin D and B vitamins, which may contribute to symptom severity. This article explores how vitamins and supplements for schizophrenia can play a role in managing symptoms, supporting brain health, and improving quality of life, while highlighting practical steps to incorporate them safely.
Understanding Schizophrenia and Nutritional Deficiencies
Schizophrenia is a chronic mental health condition characterized by symptoms like hallucinations, delusions, and cognitive challenges, often disrupting daily life. While the exact causes remain unclear, emerging research points to a connection between nutritional deficiencies and the severity of schizophrenia symptoms. Studies have found that individuals with schizophrenia frequently have lower levels of vitamins like B12, folate, and vitamin D, possibly due to dietary habits, reduced sunlight exposure, or metabolic changes associated with the condition.
Nutritional deficiencies can exacerbate symptoms by affecting brain function, neurotransmitter balance, and inflammation levels. For instance, low levels of folate and B12 are linked to elevated homocysteine, a compound that may worsen mental health outcomes. Addressing these deficiencies through vitamins and supplements for schizophrenia offers a promising adjunctive approach to traditional treatments like antipsychotics.
How Do B Vitamins Support Schizophrenia Management?
B vitamins, including B6, B8 (inositol), and B12, are essential for brain health, playing roles in neurotransmitter synthesis and cellular metabolism. Research suggests that high-dose B-vitamin supplementation can reduce schizophrenia symptoms, particularly when used alongside standard treatments. A 2017 meta-analysis of 18 clinical trials found that high doses of B vitamins significantly improved symptoms in some patients, especially those with shorter illness durations or specific genetic profiles affecting folate metabolism.
The benefits may stem from B vitamins’ ability to lower homocysteine levels, which are often elevated in schizophrenia and linked to cognitive deficits. For example, individuals with a high-functioning FOLH1 gene, which aids folate metabolism, showed reduced negative symptoms like apathy and social withdrawal when supplemented with folate and B12. However, results vary, and not all studies agree on the effectiveness, suggesting that individual differences play a significant role.
Incorporating B vitamins into a treatment plan may help manage symptoms, but the optimal dosage and combination remain under investigation. High doses should only be taken under medical supervision due to potential side effects like flushing from niacin (B3) or interactions with medications.
Can Vitamin D Improve Schizophrenia Symptoms?
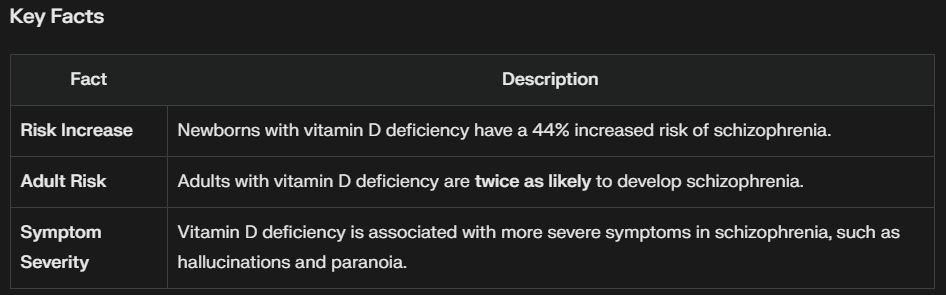
Vitamin D, often called the “sunshine vitamin,” is crucial for brain health, influencing neuroplasticity, neurotransmitter production, and inflammation regulation. Low vitamin D levels are common in schizophrenia, with a 2014 review noting that individuals with insufficient levels were more than twice as likely to have the condition. Babies born with low vitamin D also face a 44% higher risk of developing schizophrenia later in life, highlighting its role in early brain development.
A 2021 study explored vitamin D supplementation in schizophrenia patients, finding that replacing low levels improved cognitive symptoms, though effects on positive symptoms like hallucinations were less clear. Another study combining vitamin D with probiotics showed significant cognitive improvements after 12 weeks, suggesting a synergistic effect. However, the ideal vitamin D level for schizophrenia management isn’t well-defined, and some researchers argue that low levels might result from lifestyle factors, like staying indoors, rather than directly causing symptoms.
For those with schizophrenia, getting vitamin D levels checked annually and supplementing if levels are below 25 ng/mL may support brain health. Sunlight exposure and dietary sources like fatty fish can also help maintain optimal levels.
What Role Do Omega-3 Fatty Acids Play in Schizophrenia?
Omega-3 fatty acids, found in fish oil, are known for their anti-inflammatory properties and importance in brain health. A review of eight studies found that omega-3 supplementation, particularly with eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), reduced positive symptoms like hallucinations by about 25% in schizophrenia patients. Omega-3s may also protect against heart disease, a common concern for those with schizophrenia due to metabolic side effects of antipsychotics.
Interestingly, omega-3s may have preventive potential. A 2015 study of young people at high risk for schizophrenia found that only 10% of those taking fish oil supplements for 12 weeks developed the condition after seven years, compared to 40% in the placebo group. This suggests omega-3s might help delay or prevent the onset of psychosis in early stages, though more research is needed to confirm this.
A daily dose of 1 gram of omega-3s, with about 60% EPA, is often recommended by experts for schizophrenia support. This can be achieved through supplements or by eating fatty fish like salmon or mackerel twice a week.
Can Probiotics Help with Schizophrenia Symptoms?
The gut-brain axis, the connection between gut health and mental well-being, is a growing area of research in schizophrenia. Probiotics, which support a healthy gut microbiome, may influence brain function by reducing inflammation and improving nutrient absorption. A 2017 Johns Hopkins study found that probiotics reduced delusions and hallucinations in some schizophrenia patients, possibly by lowering levels of Candida albicans, a fungus often elevated in this population.
A 2019 study combining probiotics with high-dose vitamin D reported significant symptom improvements after 12 weeks, particularly in cognitive function. Probiotics may also help with gastrointestinal issues like constipation, which are common in schizophrenia due to medication side effects. Look for probiotic strains like Lactobacillus acidophilus, Bifidobacterium bifidum, and Lactobacillus reuteri for potential benefits.
While promising, the research on probiotics for schizophrenia is still in its early stages. The gut-brain connection is complex, and not all patients may experience the same benefits, especially those with a history of yeast infections.
Does N-Acetylcysteine (NAC) Offer Benefits for Schizophrenia?
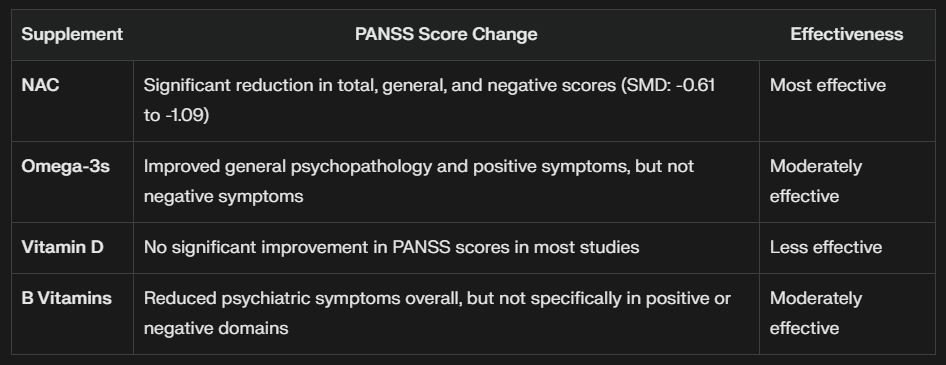
N-Acetylcysteine (NAC), an antioxidant precursor to glutathione, has shown promise in managing schizophrenia symptoms. A network meta-analysis found that NAC was more effective than folic acid, vitamin B12, or omega-3s in reducing symptom severity, as measured by the Positive and Negative Syndrome Scale (PANSS). NAC may work by reducing oxidative stress and inflammation in the brain, both of which are implicated in schizophrenia.
Studies suggest NAC can improve negative symptoms like social withdrawal and cognitive deficits, with benefits often seen after 24 weeks of consistent use. A 2022 paper noted that NAC’s effects on glutamate regulation, a neurotransmitter often dysregulated in schizophrenia, may contribute to its efficacy. However, NAC’s benefits typically take time, with little improvement seen before eight weeks.
NAC is generally well-tolerated, but its long-term effects and optimal dosing for schizophrenia need further exploration. It’s a promising supplement, but not a standalone treatment.
Notes:
- NAC (N-acetyl cysteine): Shown to be the most effective in reducing PANSS scores across various studies.
- Omega-3s: Beneficial for general psychopathology and positive symptoms but less effective for negative symptoms.
- Vitamin D: Generally found to have no significant impact on PANSS scores in schizophrenia patients.
- B Vitamins: Demonstrated some overall reduction in psychiatric symptoms, though not specifically in positive or negative symptom domains.
This comparison highlights NAC as the most effective supplement for improving schizophrenia symptoms based on PANSS score changes.
What About Other Vitamins and Supplements?
Several other supplements have been studied for schizophrenia with varying results:
- Vitamin C: As an antioxidant, vitamin C may reduce oxidative stress, which is elevated in schizophrenia. Small studies suggest it can improve symptoms, with one study noting better outcomes after eight weeks of supplementation.
- Vitamin E: Some research indicates vitamin E may help prevent tardive dyskinesia, a side effect of antipsychotics causing involuntary movements, when taken at 1,600 IU daily. However, high doses carry a risk of bleeding.
- Taurine: A 2016 study found that 4 grams of taurine daily for 12 weeks improved psychotic symptoms and depression in first-episode psychosis patients, possibly by regulating GABA and NMDA neurotransmitters.
- Ginkgo Biloba: This herb may reduce positive symptoms and antipsychotic side effects like tardive dyskinesia, but evidence is limited.
These supplements show potential, but their effects are not as well-established as B vitamins, omega-3s, or NAC. More large-scale trials are needed to confirm their benefits.
Practical Tips for Using Supplements Safely
Incorporating vitamins and supplements for schizophrenia requires a thoughtful approach. Here are some steps to consider:
- Start with a blood test to identify deficiencies, such as low vitamin D or B12 levels.
- Choose high-quality supplements with third-party testing to ensure purity and potency.
- Follow recommended dosages, such as 1 gram of omega-3s daily or 2 mg of folate with 400 mcg of B12.
- Pair supplements with a balanced diet rich in whole foods like leafy greens, fatty fish, and nuts.
- Monitor for side effects, such as gastrointestinal discomfort from probiotics or flushing from high-dose niacin.
- Track symptom changes over time to assess the effectiveness of supplementation.
Consistency is key, as many supplements take weeks to show benefits. Always integrate supplements into a broader treatment plan that includes medication and therapy.
Addressing Challenges in Supplementation
Accessing and using supplements can be challenging due to cost, lack of awareness, or skepticism about their benefits. To overcome these, look for affordable options like generic brands or bulk purchases. Educate yourself through reputable sources, but remain critical of overly optimistic claims—supplements are not a cure for schizophrenia. If motivation is an issue due to negative symptoms, set reminders or involve a supportive family member to help with consistency.
The variability in research findings also poses a challenge. Not all studies agree on the effectiveness of supplements, and individual responses differ based on genetics, illness duration, and baseline nutrient levels. This underscores the need for personalized approaches to supplementation.
Supplements as a Supportive Tool for Schizophrenia
Vitamins and supplements for schizophrenia offer a complementary strategy to manage symptoms, from reducing hallucinations with omega-3s to improving cognition with vitamin D and probiotics. They work best when addressing specific deficiencies and are most effective early in the illness. While not a replacement for antipsychotics or therapy, they can enhance overall well-being by supporting brain health and reducing inflammation.
Dietary supplements like B vitamins, omega-3s, and NAC can help address nutritional gaps and support symptom management in schizophrenia. A personalized approach, guided by blood tests and professional advice, can maximize their benefits.
Get Your Doctor’s Approval
Consult your doctor’s approval before beginning any new supplement. Even though they don’t require prescriptions, some supplements may not be safe. Your doctor will ensure there are no potential interactions with your medications or negative side effects.






